Top 7 Reasons for Back Pain while Golfing
• Can’t finish the front nine due to back pain?
• Has it been going on too long?
• Is rest not working anymore?
Frustrating, I know. Back pain is one of the top three reasons for golfers to stop playing.
If you love golf, you owe it to yourself to start treating and rehabbing your back pain today.
I know life if busy, but if you really do love the game…
• Facet Syndrome
• SI Joint Syndrome
• Disc Herniation
• Osteoarthritis
• Spinal Stenosis
• Back Spasm
• Others
FACET SYNDROME
What is Facet Syndrome?
The facets of the back are the small joints between each level of the spine. They are located all of the way up and down the spine from the sacrum to the skull.
These joints can become irritated from compression.
This irritation can create localized back pain that often gets worse when bending backwards, but every case is different.
How does Facet Syndrome create Back Pain while Golfing?
Golf is a rotational sport.
Rotation at the facets is OK to some degree, but if they move too much, then they will become painful.
Most of the rotation during a golf swing should come from the hips and the midback because in these sections, rotation is possible through their bony structure.
The low back only rotates about 5 degrees either way…so don’t make it do more.
Your core is what limits these facets from smashing into each other over and over again during your swing.
If your core, hips and midback do not function well, then you will continue to have facet pain until you address them.
Facet Syndrome Swing Mechanics
Back pain when golfing can be due to a few swing faults, so I’ll list the top three and tell you the reasons behind them.
Note that these same reasons will apply to some of the other back pain injuries, so I may just reference them quickly again in the following sections.
• Reverse Spine Angle/Tilt
• S-Posture
• Early Extension
Reverse Spine Angle and Back Pain while Golfing
Reverse Spine Angle is a term that was coined by TPI as a description of “excessive upper body backward bend or excessive left lateral upper body bend” in right-handed golfers.
The reason this is significant to many types of back pain while golfing is because it causes the lower body to be in a position for less power generation.
The upper body dominates.
In this extended, bent position, the front side abdominal muscles are “deactivated” and will not be able to protect the back against the rotational forces produced in a golf swing.
Does everyone know the mechanism for a disc injury?
Flexion and rotation under load.
What is a golf swing again? (rhetorical question)
If the disc injury doesn’t immediately leave you walking back to the club house, then over time the bony structures of the spine will continue to take a pounding, creating degenerative changes (osteoarthritis, facet irritation, spinal stenosis and more).
So, do you have a Reverse Spine Angle?
I’m not a golf pro, so I would suggest seeing one for a few lessons first. This will be money well spent if you consider that a minor coaching session or two could save you years of back pain.
There are some physical reasons for Reverse Spine Angle though too.
Your golf pro will not be able to help you through these issues.
Strength, stabilization, balance and mobility of any of the following areas could be the reason you’re shying away from using that massive lower body as a power source.
• Pelvis
• Hips
• Ankles
Also, is your trunk area strong enough to resist excessive motion in extension and bend?
It should be.
I have been very surprised by how many people that have come into my office who have back pain, but can alleviate more than half of its severity simply by engaging their trunk so they are not smashing their spine joints together in extension.
S-Posture and Back Pain while Golfing
Just imagine an S…there you have it. S-posture.
These players often look like they are sticking their butt out.
It can be seen in a down the line view or as if someone was taking a picture of you from back in the tee box.
S-posture is common in younger players, women and players who have come from other non-rotational sports.
The way S-posture creates back pain is by causing way too much extension of the lower back in this position, which is enhanced even more so with rapid rotation through the ball.
The core becomes deactivated with this over-extended arch of the back, and this sets the stage for the same possible injuries as Reverse Spine Angle (osteoarthritis, facet irritation, spinal stenosis and more).
What should your back look like when setting up?
Place a stick or club on your back, and set up into a 5-iron position. There should be minimal or no curvature between the low back and the shaft.

Facet Syndrome Rehab
Facet Syndrome rehab centers around improving the function of the front side abdominal muscles. This video explains it all very throughly.
These muscles PREVENT excessive back extension, which often leads to compression of the facets and ultimately, Facet Syndrome.
We like to start with some stretching to open the facets first.
To control excessive motion of the trunk, Pallof Press variations are a good go-to. I apologize, as this is not the exact video that I wanted. We haven’t filmed it yet.
Next, we like to stabilize the midsection with some “anti-motion” challenges. This is an Anti-Rotational Pallof Press we use to combat back pain while golfing.
We have a whole course coming out on this very topic so if you want more, you will see the course coming very soon under our “products” section.
Facet Syndrome Treatment Options
Hands-on treatment often cannot train the body to resist extension, but they can help to decompress the area.
• Stretching
• Chiropractic adjustments
• Hip mobilization
• Thoracic spine mobilization
• Deep tissue work
• Active Release Technique
• Traction
• Acupuncture
• Injections
• Oral medication
EXPECTATIONS WHEN YOU
COME SEE US IN COSTA MESA:
MORE THAN 50% IMPROVEMENT WITHIN 4-6 SESSIONS
Most Cases
MORE RELIEF WITH LESS RISK
We Only Use High Reward/Low Risk Treatments
NO RIDICULOUS LONG-TERM TREATMENT PLANS
MORE ATTENTION WITH A SKILLED GUIDE
Even Though our Costa Mesa Chiropractor are Not A "Real Doctor" 🙂
MORE THAN A TYPICAL COSTA MESA CHIROPRACTOR
No Bone Cracking Required To Feel Good
NO QUACKERY
Dr. Gonzales & Costantino Only Uses Current Evidence-Informed Methods
CLICK HERE TO BOOK YOUR APPOINTMENT WITH A COSTA MESA CHIROPRACTOR
What causes S-posture?
It can either be learned or something that your body does because of a physical compensation.
If it is learned, it can be easily fixed with some swing instruction.
If it is a physical compensation, it will take some time to fix. A few issues that can create S-posture are:
• Weak/elongated glutes, abdominals and hamstrings
• Tight/short low back muscles and hip flexors
Lower Cross Syndrome is the term many fitness and health professionals use to describe this condition.
What can you do to improve glute strength to decrease back pain while golfing?
I love this tried and true starter move. Doing it with a band is best for lower back relief and to get the glutes going. Here is a video that explains it all.
Want an advanced one?
The Barbell Hip Thruster is a safe option.
Personally, I’ve never had anyone with back pain have a negative response with this exercise, but it can be intimidating. Here’s a video on the Barbell Hip Thruster:
What can you do to improve abdominal strength to decrease back pain while golfing?
Exercises to improve abdominal wall strength are very graded. There are tons of progressions, so if my example is too hard or easy, don’t write it off.
I always start people with some coaching on how to hold the abdominal area when doing core exercise. The Lewit is the perfect starting point. Here’s a video:
Once you have the Lewit, you can advance to the Front Plank.
What can you do for thigh hip flexors to decrease back pain while golfing?
This is an interesting topic because many golfers’ hip flexors are not only tight/shortened, but weak as well.
For this reason, I will suggest a light strengthening routine in addition to stretching.
Here is the way I suggest my golfers stretch their hip flexors to decrease back pain while golfing:
After, I like to do some light strengthening.
The Supine Hip Flexion Exercise can be done for small reps and breaks when needed.
Surprisingly, it is tough for a lot of golfers.
What can you do for tight low back muscles to decrease back pain while golfing?
For this, I am all about the roller or ball…unless you want to get professional help from someone who does soft tissue work (this is the more efficient way). I’ll address this in the last section.
For at-home care, I suggest the following exercise to roll out the low back muscles with a lacrosse ball. It can be tender, and I’d suggest only doing it for a minute or so the first few times.
Early Extension and Back Pain while Golfing
Early Extension happens when you stand up as your downswing progresses through impact. Ideally, you want to remain with the same hip hinge that you had at set up all the way through impact.
Why does this matter?
To drive the ball with power you need to use your hips to create the rotational power. Extending the hips too early creates a “power leak”.
If you want to transfer your power through the ball, you need to keep it moving in rotation and not across the tee box in the wrong direction.
The resulting shots will be hooks because your hands at impact are closer to the ball than at your approach.
How does Early Extension pertain to back pain while golfing then?
Any loss of proper posture while in rotation will create abnormal forces on the components of the spine. You name it: the discs, bones and muscles will all have an altered load placed upon them leading to short term or long term back pain.
What causes Early Extension?
Just like all of the other golf faults we have gone over so far, it can either be learned or a physical compensation.
Physical issues can be:
• Limited midback mobility
• Limited hip mobility
• Weak core
• Weak gluteals
SI JOINT SYNDROME (SACROILIAC JOINT)
• Low back burning?
• Gluteal pain?
• Deep ache in the “low, low” back?
• Pain with walking and kneeling down?
These are all symptoms of SI Joint Syndrome.
An SI joint sprain is one of the secret conditions that can cause back pain when golfing because it often mimics other, more serious conditions.
If you have it, you are not alone, and it is very treatable.
Many cases of SI joint sprains can resolve within a month or less, but rehab does continue to limit re-injury.
Many people with lower back pain, have been diagnosed with SI Joint Dysfunction (or other types of SI Joint conditions) are the root of their pain.
My name is Dr. Sebastian Gonzales, sports chiropractor, and director of care at Performance Place Sports Care. As of 2021, in our past 13 years of practice, we have treated hundreds, if not thousands, of people suffering from pain in the SI joint region.
Over 9 out of 10 people who suffer from SI joint regional pain, do NOT have anything wrong with their SI joint. NOTHING.
You read it right. Most people’s SI joint pain is NOT from their SI joint being “out of place,” too tight, or too loose. Most SI joint regional pain is referred from the lower back region. We arive at this diagnosis with a very through physical exam and history taking process. We actually spend time with you and ask questions!
The good news is that spinal pain referring to the SI joint is very simple to treat without the use of medication, injections, or surgery. Our success rate has been through the roof when treating SI joint regional pain as a spinal source. Reference our Google Reviews as proof of this. 5 stars for days!
Note: You do not need to have lower back pain for your SI joint pain to be referred from your spine.
Actual SI joint pain is typically created by shearing of the SI joint, which occurs with motions like lunges, split squats, and walking (more so with longer strides).
Bending forward, backward, lifting objects, sitting posture, and sleeping position do not produce appreciable SI joint shear forces to trigger a SI Joint Dysfunction. In these situations, the root cause of your SI joint regional pain is spinal-based. Typically it is a lumbar disc, a pinched nerve or general lack of spinal stability.
Treatment of spinal referred SI joint regional pain is simple, yet it requires work on your part. We have found a blend of specific spinal stretches and stabilization exercises reduce the majority of pain within 3-4 weeks.
Complete restoration of function can come soon after. Rehabilitation requires strength training to reverse the effects of movement compensations that occur due to pain.
Here are some of the treatment methods we use in designing a long-term rehabilitation plan for SI joint regional pain:
- Specific spinal stretches
- Isometric core exercises
- Glute primers
- Hip hinge patterns (with and without weights)
- Squat patterns (with and without weights)
- Loaded carries
- Spinal and/ or mobilization (not typically required)
Recovery from SI joint regional pain is simple and based upon the hard sciences we know from rehab sciences; yet, your coach/ clinician is an artist.
Using the hard research, your clinician must regress and progress your program for your body to adapt favorably (away from the state you were in). Note: Your corrective exercises should feel challenging, but not painful in any way.
Not all doctors are created equal.
Not all SI Joint rehabilitation programs are created equal.
How you perform the exercises and stretches is MORE IMPORTANT than doing the reps.
If you need help (virtually or in-person), we can help you even if you are not close to our facility in Costa Mesa, CA. Please contact us to set up your first call. We want to help!
What is SI Joint Syndrome?
The SI joint is short for the Sacroiliac joint. I know it sounds confusing because like most other anatomical terms, it is another language.
Latin to be exact, but that doesn’t we mean we can’t break down some of the terms in the parts.
A joint is where two bones come together. There are many types of joints, such as ball and sockets and hinges.
The sacroiliac joint is where the bones of the sacrum and ilium come together.
The sacrum is the “keystone” bone between your tailbone and your back.
The ilium is one of the bones of the pelvis. You know it as where your hand goes when you “put your hands on your hips”.
There, that wasn’t so hard!
These two bones connect in your low back in a region you may recognize by the “dimples” the structures sometimes create in the lower back area.
The SI joint is the “buffer” between your hips and low back. It actually is the connecting piece to the other side of the pelvis that allows for the spread of the force of activity onto the other side of the body.
Terms you will hear surrounding articles about the SI joint are “nutation” and “counter-nutation”.
Nutation simply means movement of the top part of the sacrum forward on the other sides of the joint (ilium bones).
Counter-nutation means movement in the opposite direction.
Both of these motions allow for the dissipation of forces through the body to limit pain.
Here is a great article on the topic:
https://breakingmuscle.com/learn/why-your-si-joint-is-such-a-pain-and-4-exercises-to-fix-it
How does SI Joint Syndrome create Back Pain while Golfing?
The SI joint can become irritated when it is too “loose” or over-compacted.
Hypermobility is the term most people will use when talking about the “loose” cases.
Fixation or hypomobility is used in the compaction cases.
What kind do you have?
Examination can tell for sure, but with golfers, oftentimes it is the compaction variety on the trailside, but you can have either type.
It depends on your overall health, how physically fit you are and if you have any past injuries.
What golf swing mechanics are involved in SI Joint Syndrome?
Not surprisingly, the same swing faults can affect golfers in the SI joints the same as in other back conditions.
Please read the section on Facet Syndrome at the top of this page for full details on this section.
• Reverse Spine Angle/Tilt
• S-Posture
• Early Extension
• Sway
• Slide
How to rehab SI Joint Syndrome?
Think of SI Joint Syndrome as not having enough support around the joint…or it being too “loose”.
Or it can be compacted…I know, it’s complicated that it can be either.
These joints don’t move a ton as it is, but if they are required to move more than they normally do, they will become sprained just like an ankle.
SI Joint pain can treated and rehabbed very easily when it is caught early.
How?
Improving the function of the joints around the region via improving:
• Range of motion
• Strength
• Endurance
• Movement patterns
The hip and trunk (regions below and above) are the first ones to deal with. Here are some of our favorite hip exercises for SI joint pain.
These are good starter exercises, but what we really need to improve is muscle imbalance around the joint while your feet are on the ground. For this, we need to use closed chain exercises such as:
• Deadlifts
• Squats
• Lunges
• Ext.
Why?
Weakness of the posterior chain, specifically the glutes and hamstrings, needs to be corrected since these muscle groups assist the SI joint in doing its job of transferring loads.
Dr. Stewart McGill, one of the experts in back pain, put it in simple terms when he said, “if the SI joint is not working properly, the force is going to go somewhere”. This time, it could be your back.
What treatments are available for SI Joint Syndrome?
Here are some treatments I strongly suggest to control pain associated with SI Joint Syndrome:
• Stretching
• Chiropractic adjustments
• Hip mobilization
• Thoracic spine mobilization
• Deep tissue work
• Active Release Technique
• Traction
• Acupuncture
• Injections
• Oral medication
If you are looking for a quick way to relieve pain from SI joint dysfunction, I have found the following rolling technique to be very helpful for short-term relief.
If you have a baseball or a lacrosse ball you’re in luck. This should only take a few minutes.
DISC HERNIATION
• Pain with bending forward?
• Worse in the morning?
• Can’t bend over to pick up your ball?
All of these are possible signs and symptoms of a disc herniation. Disc injuries are very frustrating to golfers since it can literally stop you in your tracks.
Luckily, if you rehab and treat it when it is small, you can avoid surgery and time away from the course.
Read this article and learn the facts about what a disc injury is and how it is often rehabbed.
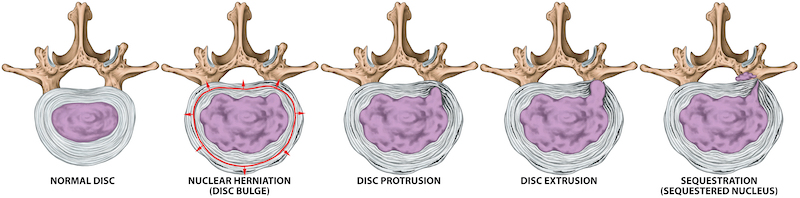
What is a Disc Herniation?
A disc herniation is when the “jelly donut” in a section of your back has become torn or when the “jelly” begins to come out.
These discs are softer than bone, and as such, can be ripped resulting in pain.
There are different severities of disc injuries (best to worst)
• Protrusion
• Prolapse
• Extrusion
• Sequestration

Disc Herniations & Golfing
Disc herniations tend to present themselves during golf because golf is a rotational sport, it is prime to cause disc injuries.
Disc injuries occur from flexion and rotation.
They occur more commonly when the golfer has poor core strength and hip mobility.
Wondering if your core would be considered weak?
If you hesitate to answer, “yes” to the following question, then I would be highly suspicious.
Do you do a core routine (on the ground) for more than 20 minutes a week or weightlift for more than an hour a week?
Hesitation means your core is probably an issue.
What golf swing mechanics are often involved in a Disc Herniation?
I covered these extensively in the Facet Syndrome section, but I will simply list them here so I am not too redundant.
• Reverse Spine Angle/Tilt
• S-Posture
• Early Extension
These are your top three, but there are many more.
How to rehab a Disc Herniation?
Disc injuries really do not like spinal flexion.
If you still don’t understand why disc injuries get worse with certain motions, like flexion, you need to watch this video to its entirety.
Spinal flexion is the movement of bending forward to touch your toes, doing a yoga forward fold, picking up your ball, etc.
Granted, you could be doing these with the hips, which would be the correct way, but if you are adding even small amounts of lumbar spine flexion, then your discs will become irritated.
So how do we rehab it?
We do it in extension or neutral…and add in flexion later.
The stabilizer muscles of the spine do not function well if you are in pain. It becomes a vicious cycle, and for rehab, we keep you in a non-painful position and strengthen the stabilizer groups without a pain stimulus.
Here is an exercise series I like to suggest for disc injury patients to manage the pain quickly. If you don’t feel better doing this, you may not have a disc injury.
And while we are talking about “if this, then that” scenarios, if you have back pain with a drop foot, bowel or bladder complications and/or two-sided pain, then you need to go to the ER RIGHT NOW. These are all legitimate, medical emergencies. You don’t want to mess around with any of these situations…seriously.
What treatments are available for a Disc Herniation?
in the video I linked to above covers a few of my favorite corrective exercises and stretches for low back disc herniations. If you didn’t watch, you should before you even consider the treatment options below. Disc herniations do not always need surgery, BUT some do. If you read the last section, you saw the disclaimer on the medical emergency.
Here are some treatments I have suggested for disc herniations:
• Stretching
• Chiropractic adjustments
• Hip mobilization
• Thoracic spine mobilization
• Deep tissue work
• Active Release Technique
• Traction
• Acupuncture
• Injections
• Oral medication
• Surgery
OSTEOARTHRITIS
• Deep backache?
• Stiffness?
• Worse as it gets colder?
Osteoarthritis is an extremely common condition with older golfers. By older, I mean the 50 plus variety.
If you have been told you have arthritis, it does not have to be a death sentence. Many people actually seem to have this mindset.
“There is nothing you can do for me…it is arthritis.”
Wrong.
Your arthritis will not change, that is correct, but the way you feel and play can.
In this article, you should come away with a better understanding of how to combat age- related decline of your golf game.
What is Osteoarthritis?
Osteoarthritis or “Arthritis” is known as the “old age” type of arthritis.
Everyone gets it to some degree.
As the body ages, the joints with the most abnormal wear patterns start to degrade.
Bony formations occur in these areas as the body is remodeling due to the abnormal wear patterns.
This form of arthritis can occur anywhere in the body and more commonly, in areas where you have had a past injury or trauma.
Osteoarthritis & Golfing
Abnormal wear patterns on joints are not normal naturally. They’ve occurred as your body has compensated.
If you had a hip or knee injury (small or large) in the past, afterwards, you began to move differently.
You changed your swing, the way you walked the course, stood, sat…you name it.
These movement changes created abnormal wear on the back and told your body to create new bone in that region which over time has led to arthritis.
How can we prevent arthritis then?
• Don’t ignore old injuries
• Keep rehabbing even though you feel better
• Strengthen your body
• Improve your swing mechanics
Simply put, be responsible. Your old injuries will come back to haunt you in one way or another if you’re not.
Osteoarthritis Rehab
Osteoarthritis itself is not fixable with rehab. BUT how you feel is.
We suggest focusing on mobility of the:
• Hips
• Ankles
• Midback
And strengthening of the:
• Core
• Hips
• Legs
Sure, the rest of the body is important too, but these are great, “bang-for-your-buck” regions.
Eventually, moving to loaded complex motions like squatting, deadlifting, pushing, pulling and carries are great for a whole body session.
Mobility
Here is a stretching series (video) I recommend for some of my arthritis clients:
Strengthening
Strengthening does not have to be complicated. Just get out and walk, pick up leaves, squat down to look at ants and so on. Using gravity and body weight is an excellent starting point. General movement gets the body lubricated up and loads the joints and muscles in a low risk/ high reward way.
Osteoarthritis Treatment Options
Any treatments that can decrease pain associated with arthritis are great when used in combination with rehab therapy.
• Stretching
• Chiropractic adjustments
• Hip mobilization
• Thoracic spine mobilization
• Deep tissue work
• Active Release Technique
• Traction
• Acupuncture
• Injections
• Oral medication
EXPECTATIONS WHEN YOU
COME SEE US IN COSTA MESA:
MORE THAN 50% IMPROVEMENT WITHIN 4-6 SESSIONS
Most Cases
MORE RELIEF WITH LESS RISK
We Only Use High Reward/Low Risk Treatments
NO RIDICULOUS LONG-TERM TREATMENT PLANS
MORE ATTENTION WITH A SKILLED GUIDE
Even Though our Costa Mesa Chiropractor are Not A "Real Doctor" 🙂
MORE THAN A TYPICAL COSTA MESA CHIROPRACTOR
No Bone Cracking Required To Feel Good
NO QUACKERY
Dr. Gonzales & Costantino Only Uses Current Evidence-Informed Methods
CLICK HERE TO BOOK YOUR APPOINTMENT WITH A COSTA MESA CHIROPRACTOR
SPINAL STENOSIS
What is Spinal Stenosis?
Stenosis means “narrowing”.
Narrowing of what?
Well, if it is “central stenosis”, then it is the center of the spinal column.
“Neural Foraminal Stenosis” is a narrowing of the holes that the spinal nerves leave the spine through.
Each can have a different symptom pattern.
Why does the narrowing happen?
The space could be narrowed for a few reasons.
• Enlargement of the bones in the area
• Hypertrophy (enlargement) of a ligament
• Tumor or space occupying lesion
Spinal Stenosis & Golfing
Stenosis is much like osteoarthritis. It creates back pain while golfing because of abnormal wear patterns.
Someone with stenosis can experience the following, whereas a non-stenosis/arthritis golfer will not:
• Bony pinch points
• Compression of the spinal cord or nerve roots
• Spasm of the muscles around the spine
To know more about stenosis, please read the section on arthritis because stenosis is often advanced arthritis within a section of the spine.
What golf swing mechanics are often involved in Spinal Stenosis?
Not surprisingly, the same swing faults can affect golfers in Spinal Stenosis as with other back conditions. Please read the section on Facet Syndrome at the top of this page for full details on this section.
• Reverse Spine Angle/Tilt
• S-Posture
• Early Extension
• Sway
• Slide
Spinal Stenosis Rehab
I’ll be honest with you. Personally, I’ve had little success rehabbing patients with stenosis.
I have had excellent outcomes with many other types of injuries.
Disc injuries, back spasms, and Facet Syndrome all have much better outcomes than Spinal Stenosis.
For this reason, I will not supply any guidance on this topic, BUT in theory, rehab would follow the same methodology as arthritis.
The only difference is it is harder to get the person into a position of comfort to allow the stabilizer muscles to start working.
If there are any other healthcare professionals out there reading this article, I would love to have your input to help everyone out.
Spinal Stenosis Treatment Options
I’ll default to my last statement on treatments. If anyone has long-term, magical treatment for those with stenosis, speak up (supply some research too, if you can) and I will post it referencing you in this section.
BACK SPASM
• Tight back after golfing?
• Improves with heat?
• Improves with rest?
These are just some of the signs and symptoms of muscular back spasms that can occur with golfing.
Spasms can be extremely painful, but they can also be very easy to treat.
Of all of the conditions that I’ve written about on this page, this is one of the better ones to have.
In this article, you should come away with some great information about back spasms while golfing and how to combat them.
What Is A Back Spasm?
A spasm is when a muscles contracts and tightens. The reason why these particular muscles are spasming can range from being very benign or super serious.
For this reason, when you do experience spasms in the back, you should still have an exam with a doctor to make sure that’s all they are.
Any of the muscles of the body are capable of becoming spasmatic.
So, why are the ones in your back tightening now?
You’ve probably forced them to do too much over the last few days or week.
Back Spasms & Golfing
When golfing, the muscles of the trunk and back go through some very extreme motions.
I would gamble that your golf swing is the fastest motion you do all week. Acceleration and deceleration are reasons for muscles to spasm.
During your swing, the muscles of the trunk have two jobs:
• Produce motion to drive the ball
• Protect your spine
If you are not conditioning yourself all week for golf and expect to feel great after playing 18, you’re fooling yourself.
Be an athlete, not a “weekend warrior”.
What golf swing mechanics are often involved in a Back Spasm?
Please read the section on Facet Syndrome at the top of this page for full details on this section.
• Reverse Spine Angle/Tilt
• S-Posture
• Early Extension
• Sway
• Slide
Back Spasm Rehab
Rehabbing spasms in the back begin with decreasing pain in the area. If you are dealing with spasms right now, forget stretching and massaging. Watch this video and follow along.
Rehabilitation, stretching and building strength tends to work best if you settle the spasm quickly rather than trying to work through it. If this exercise works for you, contact us and we can help you design a custom rehab program.
Back Spasm Treatment Options
Here’s a whole list. Wondering what is the best for you? Everyone is different.
I would go from the least invasive to the most. Soft tissue work is a very safe place to start.
• Stretching
• Chiropractic adjustments
• Hip mobilization
• Thoracic spine mobilization
• Deep tissue work
• Active Release Technique
• Traction
• Acupuncture
• Injections
• Oral medication
Chronic Low Back Pain & Golf
I’m sure all of the above therapies sound awesome if you are dealing with back pain but remember movement and staying strong are extremely important to your long-term improvement.
I apologize for the echo in this video but the content is good. I am talking about a study on exercise and chronic low back pain… did it make it better, worse or the same?
SCARY LOW BACK CUASES
I have written this section to let you know that there are other conditions that could be causing back pain.
It’s my responsibility to inform you.
Here is a short list (some are scary):
• Malignant tumor
• Non-malignant tumor
• Fractures
• Pregnancy
• Organ pathology
• Infection
• Endometriosis
• Medication side effects
• Others
You need to always have a proper exam and recommendation before starting any rehab. Be responsible and see someone in person first.