Sciatica: All You Need To Know To Get Better
This sciatica article was updated in 2021, which means there is no old, outdated information. I’d encourage you to read the treatment section at the end of the article, as it will include critical information that is not often in other sciatica articles.
Hi, I’m Sebastian Gonzales, director of care at Performance Place Sports Care in Costa Mesa CA.
If this article seems to long for you, just watch this Youtube video I made. It’s 25 mins and fully informative

What Does Sciatica Feel Like?
Sciatica can present in a variety of different way, yet we can start with a textbook symptom presentation and go from there:
- Pain: Pain starts in the lower back and intensifies as it travels down the backside of the thigh, to the leg/ calf region, and finally to the bottom of the foot
- Numbness: Numbness of the back of the leg is common but not a requirement associated with sciatica. Leg weakness and/or tingling is more common in the early stages. This may feel like “heaviness” or a “loss of power.”
- Single-sided: Sciatica is a single-sided condition, meaning if you have symptoms on both legs at the same time, you do not have sciatica. Pain in two legs is an indication of another possible diagnosis list.
- Position/ posture dependent: Sciatica is typically position or posture induced, meaning you can feel normal in one position or activity and intense pain in another, all in the same day. Positions that tend to trigger sciatica is sitting, bending forward, hamstring stretching, twisting, rolling in bed, sit-ups, deadlifting, deep squats, and/or walking.
Sciatica Is the Symptom of an Underlying Medical Condition
Sciatica is a symptom of the main diagnosis. Sciatica (meaning leg pain) is not a “true diagnosis;” it is a symptom. An example is sweating is a symptom of a heart attack. Sciatica/ unilateral leg pain is found with these diagnoses:
- lumbar disc injury/ “thrown out back”
- lumbar spinal radiculopathy/ “pinched nerve”
- central canal stenosis
- foraminal stenosis
- tumor
- spondylolisthesis
- spinal infection
- Piriformis Syndrome
Contrary to popular belief muscle spasms, tight hamstrings, and hip flexors do not cause sciatica, yet they are often found as an associated symptom in most people.
SI Joint Dysfunction does not tend to refer to the leg in the form of sciatica (beyond the knee joint), but the lumbar spine can be affected simultaneously creating sciatica.
A strong majority of the time, people experience sciatica due to a lumbar disc injury or a pinched spinal nerve.

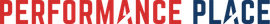
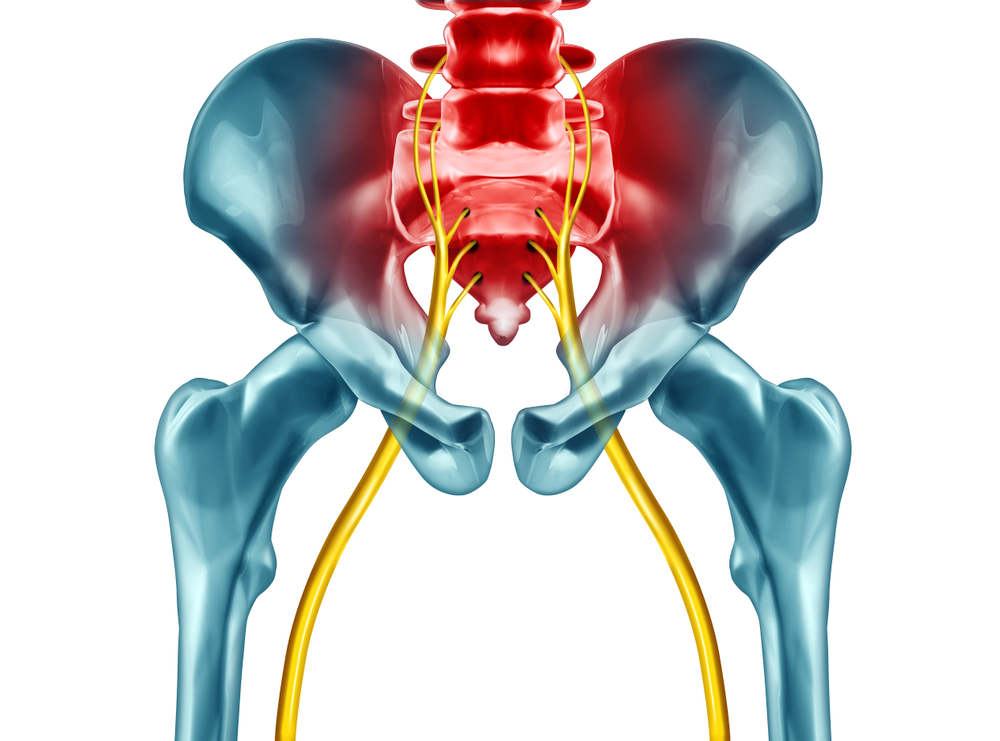
The Anatomy Of Buttocks & Leg Pain
The sciatic nerve is the large nerve of the body, composed of multiple spinal nerve root levels. It passes through the pelvis, under the hip external rotators (including the piriformis), through the hamstrings before splitting into two tributary nerves (tibial and common peroneal nerves).
The tibial nerve travels down the backside of the leg/ calf to the bottom of the foot. This branch is most commonly affected in sciatica. Sciatica in this region mimics plantar fasciitis, heel pain, metatarsalgia, and calf cramps.
The common peroneal nerve passes on the outer part of the knee, to the side of the shin, to the top of the foot, and even between the webbing of the toes. Sciatica in this region mimics peroneal tendonitis, shin splints, and ankle sprains oddly.
When It Is Serious?
Sciatica should be taken seriously and you should always be examined by a qualified medical professional. This can be a sports chiropractor, a doctor of physical therapy, a medical doctor, an orthopedic doctor, or a neurologist.
Massage therapists and personal trainers are not qualified, nor trained, to diagnose sciatica (sorry guys I love your work, no offense.)
Note: Massage and personal training can be critical aspects of a treatment plan, just not the diagnosis aspect.
A thorough history and physical examination must be taken, this may or may not include an image like an X-ray or MRI. Contrary to popular belief, X-ray and MRI are not required to diagnose sciatica, nor start treatment! This will require about 30-60 minutes or more of the doctor’s time.
Red flags you should be concerned about are:
- Changes in urinary stream
- Having trouble buttoning up shirts, tying their shoes, dropping objects, frequent typos when texting
- Unrelenting headaches
- Change of vision or hearing
- Difficulty with breathing or shortness of breath
- Weakness in hand or arm
- Frequency or urgency of urination
- Changes in bowel function
- Numbness in the shape of a saddle between their thighs
- Recent inability to use their foot (tripping on rugs and objects)
- Recent unwanted weight loss
- Fever of unknown origin
- Night sweats
- Increased pain at night time
- History of cancer
- Progressively getting worse at a quick rate and an inability to find a single position where the pain is reduced
These are just a few of the red flag questions your healthcare provider should be asking about when you report for a full examination. Here’s the rest of the list.
How To Get Rid Of Sciatica?
First and foremost, know that well over 9 out of 10 people with sciatica do not require medication, injections, or surgery to return to normal life.
While each treatment provider may design your treatment plan slightly different, best relief generally will include some of the following:
- Low back stretching
- Hip mobility
- Glute exercises
- Isometric core exercises
- Walking
- Resets: Coaching you into pain-free positions
- Coaching of painful to become pain-free
- Resistance training
Many people believe yoga, stretching, chiropractic adjustments, acupuncture, ice, heat, foam rolling, diet, pilates, and much more are the answer for their sciatica problem. Personally, I do not recommend these often and we get amazing results. In fact, daily walking is the cheapest and most effective form of sciatica treatment.
It’s important to note, a treatment that may help one person’s sciatica will make another’s worse. Your treatment plan should be custom based upon your diagnosis (remember sciatica is not the primary diagnosis). A skilled provider will be able to show you the right way to feel better.
Medicine is based upon the hard sciences, it is also an art.
Your provider is the artist. Make sure they are willing to show you how to perform your exercises. No exercise or stretch should hurt after you’re done. If it does, your provider can help you select a better option for you.
If you want help from us, we offer in-person or virtual treatment that can yield amazing results. We are in Costa Mesa CA, yet we invite you to contact us via email on the website to discuss your case.